What is Peripheral Neuropathy?
Peripheral neuropathy refers to damage or dysfunction of the peripheral nerves—the vast network that transmits signals between the central nervous system (brain and spinal cord) and the rest of the body. These nerves control everything from muscle movement to sensation and even automatic functions like heart rate and digestion.
When these nerves are damaged, communication between the brain and body becomes disrupted, leading to a wide range of symptoms. Peripheral neuropathy is not a single disease but a symptom of many possible conditions.
Common Causes and Risk Factors
Peripheral neuropathy has many potential causes. Understanding the underlying reason is crucial for effective treatment.
Leading Causes
- Diabetes Mellitus: The most common cause in the developed world, responsible for up to 50% of cases (Mayo Clinic).
- Alcohol Abuse: Chronic alcohol consumption can lead to vitamin deficiencies and nerve damage.
- Vitamin Deficiencies: Particularly B vitamins (B1, B6, B12), folate, and vitamin E.
- Infections: Such as Lyme disease, HIV/AIDS, shingles (herpes zoster), and hepatitis C.
- Autoimmune Disorders: Including rheumatoid arthritis, lupus, and Guillain-Barré syndrome.
- Medications: Some chemotherapy drugs, antibiotics, and statins.
- Inherited Disorders: Like Charcot-Marie-Tooth disease.
- Trauma or Injury: Physical injury to nerves through accidents, surgery, or repetitive stress.
Risk Factors
- Age (risk increases with age)
- Family history of neuropathy
- Chronic diseases (kidney, liver, thyroid disorders)
- Exposure to toxins (heavy metals, industrial chemicals)
Recognizing the Symptoms
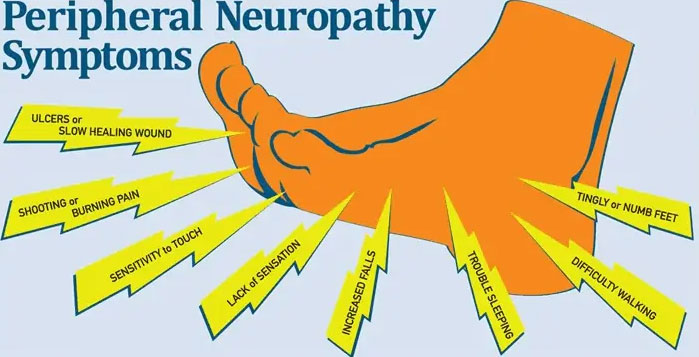
Symptoms of peripheral neuropathy can vary widely depending on the type of nerves affected—sensory, motor, or autonomic.
Common Symptoms
- Numbness or tingling (pins and needles) in the hands or feet
- Burning, stabbing, or shooting pain
- Muscle weakness or cramps
- Loss of coordination or balance
- Sensitivity to touch (even light touch can be painful)
- Changes in skin, hair, or nail health
- Digestive issues, dizziness, or abnormal sweating (if autonomic nerves are involved)
Symptoms often start gradually and may worsen over time. Early recognition is key to preventing further nerve damage.
How Peripheral Neuropathy is Diagnosed
A thorough diagnosis is the first step in demystifying peripheral neuropathy: your comprehensive guide to relief, recovery, and resilience. Accurate diagnosis ensures targeted treatment.
Diagnostic Process
- Medical History & Physical Exam: Your doctor will ask about symptoms, medical history, lifestyle, and possible exposures.
- Neurological Exam: Tests for reflexes, muscle strength, sensation, and coordination.
- Blood Tests: To check for diabetes, vitamin deficiencies, thyroid issues, infections, or autoimmune markers.
- Nerve Conduction Studies & Electromyography (EMG): Measure electrical activity in nerves and muscles.
- Imaging: MRI or CT scans may be used to rule out other causes.
- Nerve Biopsy: Rarely, a small piece of nerve tissue is examined under a microscope.
Expert Tip: Early diagnosis can prevent progression and improve outcomes. If you notice symptoms, consult your healthcare provider promptly.
Relief: Medical and Lifestyle Treatments
Relief from peripheral neuropathy is possible with a combination of medical interventions and lifestyle adjustments. The most effective approach is individualized, based on the cause and symptoms.
Medications and Conventional Therapies
- Pain Relievers: Over-the-counter options (acetaminophen, NSAIDs) for mild pain; prescription medications for severe cases.
- Antidepressants: Certain types (amitriptyline, duloxetine) can relieve nerve pain even in non-depressed patients.
- Anticonvulsants: Medications like gabapentin and pregabalin are commonly prescribed.
- Topical Treatments: Capsaicin cream or lidocaine patches can help localized pain.
- Treating Underlying Conditions: Managing diabetes, correcting vitamin deficiencies, or stopping offending drugs can halt or reverse nerve damage.
Physical Therapy and Exercise
- Physical Therapy: Customized exercises help maintain strength, mobility, and balance.
- Occupational Therapy: Teaches strategies for daily living and adapting to physical changes.
- Low-Impact Exercise: Walking, swimming, or yoga can improve circulation and reduce pain.
Diet and Nutritional Support
- Balanced Diet: Emphasize whole grains, lean proteins, fruits, and vegetables.
- Vitamin Supplementation: Especially B vitamins if deficient.
- Limit Alcohol and Processed Foods: Reduces inflammation and supports nerve health.
Practical Advice:
If you have diabetes, work with a registered dietitian to control blood sugar and reduce neuropathy risk.
Complementary and Alternative Approaches
- Acupuncture: Some studies show benefit for pain relief.
- Massage Therapy: May improve circulation and reduce discomfort.
- Transcutaneous Electrical Nerve Stimulation (TENS): Delivers mild electrical impulses to disrupt pain signals.
- Mind-Body Techniques: Meditation, mindfulness, and relaxation exercises can help manage chronic pain.
Recovery: Managing and Reversing Neuropathy
While not all cases of peripheral neuropathy are reversible, many people achieve significant improvement with the right approach.
Steps Toward Recovery
- Identify and Treat the Underlying Cause: For example, strict blood sugar control in diabetes can slow or stop progression.
- Adhere to Treatment Plans: Consistency with medications, therapies, and lifestyle changes is key.
- Monitor Progress: Keep a symptom diary and report changes to your healthcare provider.
- Regular Follow-Up: Adjust treatments as needed for optimal results.
Real-Life Example
Maria, age 58, was diagnosed with diabetic neuropathy. By working closely with her endocrinologist, she improved her blood sugar control, attended physical therapy, and adopted a Mediterranean-style diet. Over 18 months, her symptoms reduced significantly, and she regained much of her lost mobility.
Can Neuropathy Be Reversed?
- Early-stage neuropathy caused by vitamin deficiencies, medication side effects, or infections may be reversible if the cause is treated promptly.
- Chronic cases (especially long-standing diabetes or inherited forms) may not be fully reversible, but symptoms can often be managed and progression slowed.
Authoritative Source:
For more on neuropathy recovery, visit the National Institute of Neurological Disorders and Stroke (NINDS).
Resilience: Living Well with Peripheral Neuropathy
Building resilience means adapting to life with neuropathy while maximizing quality of life and independence.
Coping Strategies
- Education: Learn about your condition and stay informed about new treatments.
- Support Networks: Join neuropathy support groups or online communities for shared experiences and advice.
- Home Safety: Reduce fall risks by securing rugs, installing grab bars, and using assistive devices if needed.
- Mental Health: Address anxiety or depression proactively—chronic pain can affect mood.
Practical Tips for Daily Living
- Foot Care: Inspect feet daily for injuries, especially if you have diabetes.
- Comfortable Footwear: Wear well-fitting shoes with cushioning and support.
- Routine: Establish regular sleep, meal, and exercise schedules.
- Adaptive Devices: Use canes, walkers, or other aids as needed for mobility and safety.
Frequently Asked Questions
What is the best treatment for peripheral neuropathy?
The best treatment depends on the underlying cause. For many, a mix of medications, physical therapy, and lifestyle changes offers the most relief.
Can peripheral neuropathy be prevented?
Some forms can be prevented by controlling diabetes, avoiding toxins, moderating alcohol, and maintaining a healthy lifestyle.
How long does it take to see improvement?
Improvement varies. Some people notice relief within weeks of starting treatment; others may require months of consistent management.
Is exercise safe for people with neuropathy?
Yes, with guidance from a healthcare provider or physical therapist. Low-impact activities are generally safest and most beneficial.
Conclusion
Demystifying peripheral neuropathy: your comprehensive guide to relief, recovery, and resilience is about empowering you with knowledge, practical tools, and hope. While peripheral neuropathy presents real challenges, advances in medical care, lifestyle strategies, and community support make it possible to manage symptoms, pursue recovery, and live a fulfilling life. Always consult your healthcare provider for personalized advice and stay proactive in your journey toward nerve health and resilience.
This article is for informational purposes only and does not substitute for professional medical advice. For diagnosis and treatment, consult your healthcare provider.
